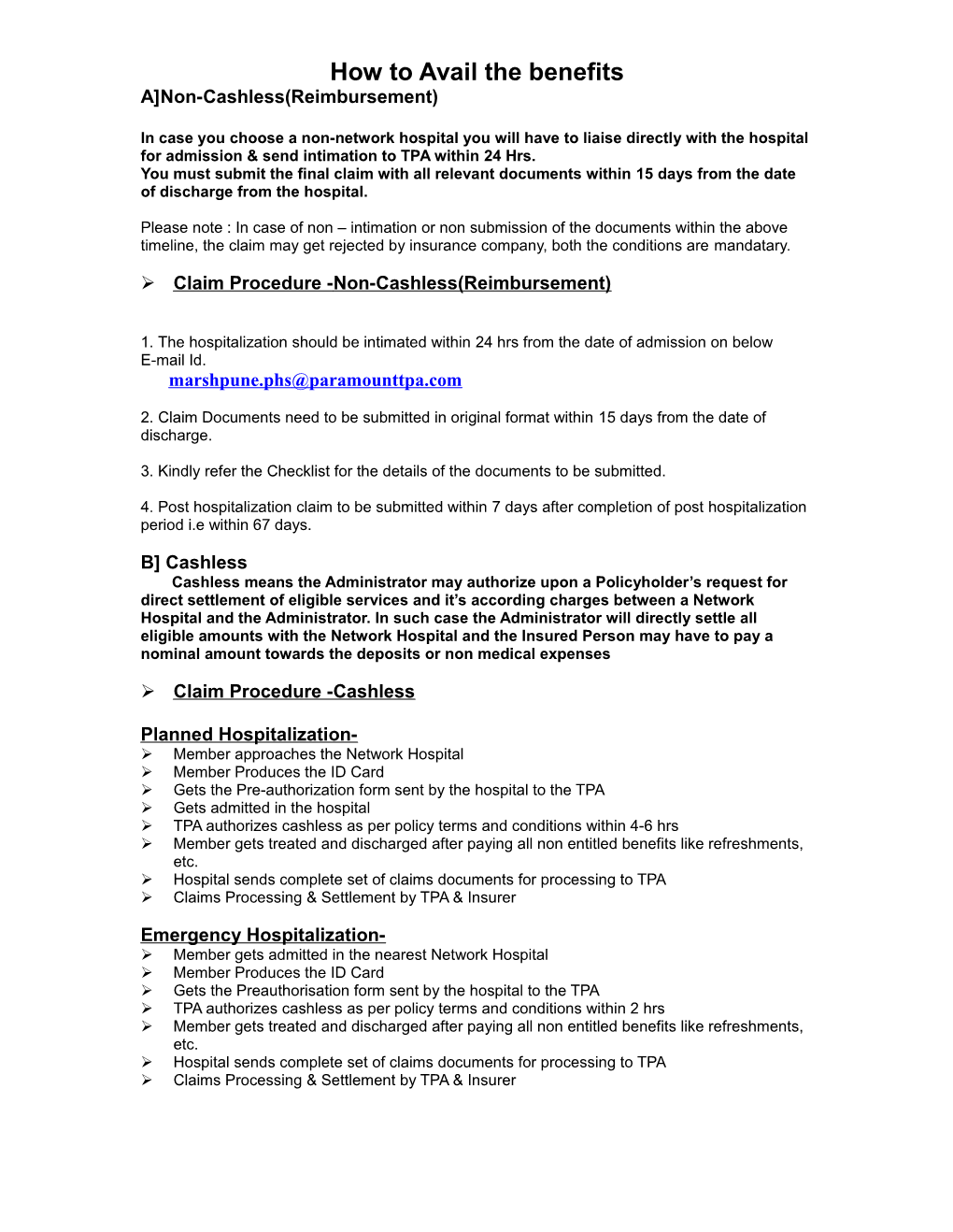
How to Avail the benefits
A]Non-Cashless(Reimbursement)
In case you choose a non-network hospital you will have to liaise directly with the hospital for admission & send intimation to TPA within 24 Hrs.
You must submit the final claim with all relevant documents within 15 days from the date of discharge from the hospital.
Please note : In case of non – intimation or non submission of the documents within the above timeline, the claim may get rejected by insurance company, both the conditions are mandatary.
Claim Procedure -Non-Cashless(Reimbursement)
- The hospitalization should be intimated within 24 hrs from the date of admission on below
E-mail Id.
- Claim Documents need to be submitted in original format within 15 days from the date of discharge.
- Kindly refer the Checklist for the details of the documents to be submitted.
- Post hospitalization claim to be submitted within 7 days after completion of post hospitalization period i.e within 67 days.
B] Cashless
Cashless means the Administrator may authorize upon a Policyholder’s request for direct settlement of eligible services and it’s according charges between a Network Hospital and the Administrator. In such case the Administrator will directly settle all eligible amounts with the Network Hospital and the Insured Person may have to pay a nominal amount towards the deposits or non medical expenses
Claim Procedure -Cashless
Planned Hospitalization-
Member approaches the Network Hospital
Member Produces the ID Card
Gets the Pre-authorization form sent by the hospital to the TPA
Gets admitted in the hospital
TPA authorizes cashless as per policy terms and conditions within 4-6 hrs
Member gets treated and discharged after paying all non entitled benefits like refreshments, etc.
Hospital sends complete set of claims documents for processing to TPA
Claims Processing & Settlement by TPA & Insurer
Emergency Hospitalization-
Member gets admitted in the nearest Network Hospital
Member Produces the ID Card
Gets the Preauthorisation form sent by the hospital to the TPA
TPA authorizes cashless as per policy terms and conditions within 2 hrs
Member gets treated and discharged after paying all non entitled benefits like refreshments, etc.
Hospital sends complete set of claims documents for processing to TPA
Claims Processing & Settlement by TPA & Insurer